

Why should you be concerned with the ergonomics of the operatory? Ergonomics is a great buzzword, but not many doctors are energized by it.
Too bad.
Because paying attention to establishing an ergonomic environment in the operatory can dramatically enhance your physical well-being and make you feel much more relaxed and refreshed at the end of the workday. So, how do you create this ideal operator?
Read on.
Especially with operatories or clinical exam/treatment rooms, form follows function because active movement and treatment occur in these rooms.
“Form follows function” is a time-honored phrase in any design process, but most dental and medical offices are designed so that function follows form. Who would argue that frequently the doctor will purchase the desired equipment and cabinetry before planning and designing the facility, and the office is then designed around the equipment?
Hold the phone! The staff, not the equipment, is the most important thing in the room. The design should revolve around the people and only then should a decision be made as to how to implement the equipment and cabinetry.
This process is the true meaning of form follows function. Any bur was not designed because the designer wanted to create a pretty shape, but rather because it will create a margin, reduce an occlusal surface, open a contact, or perform an osteotomy. The bur is designed to perform a specific function and it was shaped accordingly. Able designers insist that form must follow function and this principle produces truly beautiful finished products.
This principle should also be observed when considering the integration of high-tech components into the design of the office. Often, high-tech equipment clutters operatories and offices because no thought has been given as to how or when it will function and whether it requires storage in the clinical treatment room or a separate parking space (see Chapter VII for more information on technology planning).
Clinical treatment room or dental operatory circulation must be considered, that is, the movement of the doctor, staff, and patient. In terms of design for the medical and dental office, everything that will be described complies with the Health Insurance Portability and Accountability Act (HIPAA).
When operatory circulation was initially evaluated ergonomically, dental chairs were placed in a large empty room and the doctors and assistants were then their traffic patterns were charted.
When the dental personnel were totally unhindered or unobstructed in their movement, they chose the path of least resistance and least distance; a pattern of movement was established that was parallel to the long axis of the dental chair. The subjects tended to travel along these lines or paths parallel to the dental chair over 90% of the time. If this is the pattern in which staff travels, it suggests that people will always choose the path that offers the least resistance and the path that reduces physical stress.
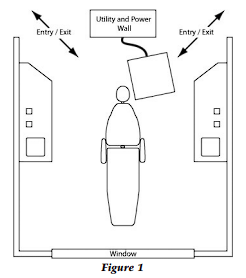
This information indicates that walls may be constructed for privacy where people do not travel and where there is no equipment. Therefore, the logical configuration of the operatory is a dual rear entry with easy ingress and egress for the individual doctor and assistant (Fig. 1).
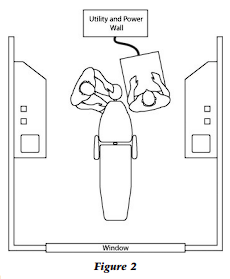
In order to achieve a physically non-damaging work environment, i.e., an ergonomically favorable environment, the dental operatory must be designed with the doctor, patient, and assistant in the seated position. That is, the patient is reclined, the doctor is seated at the nine to twelve o’clock position relative to the head of the patient, and the assistant is situated so that her left hip is adjacent to the patient’s left shoulder and her eye level is eight inches higher than that of the doctor (Fig. 2).
With this positioning the assistant can visualize the operating field and efficiently pass all instrumentation to the doctor. Instrumentation and materials should be managed and controlled by the assistant with the doctor receiving, using, and returning all equipment and materials to the assistant with the “four-handed instrument-passing” technique. Employing “four-handed dentistry” should result in minimal class I, II, and III movements for the doctor during the treatment procedure.
There are five ergonomic classes of movement designed to communicate which movements are desirable and which movements are damaging to the skeleton and musculature. Class one movement is finger movement only. Class two movement involves the wrist and hand. Class three involves the elbow in adduction. Class four involves abduction or elevation of the elbow and shoulder, which, on a repetitive basis, can be very damaging and lead to inflammatory joint disease. Class five movements involve rotation of the trunk at the waist and are to be avoided whenever possible.
With the assistant managing and passing all instruments and materials, the operatory should necessarily be designed around the physical dimensions and functional movements of the assistant. The objective is to achieve a doctor’s range of motion that goes no further than class III movement and the assistant’s range of motion go no further than class IV during 80% of the procedure time.
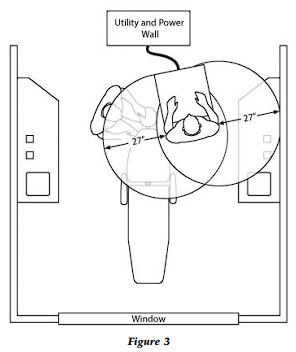
Therefore, the 27-inch reach of the average female, from the shoulder girdle to the tip of the fingers, is a key element in operatory dimensions. This dimension will indicate the placement of instrumentation and materials that are primary and secondary in usage during the dental procedure.
With the dental assistant in position beside the patient, two circles can be drawn with a 27-inch radius with the circle centers placed at the assistant’s shoulders (Fig. 3). Any area within the frontal hemispheres of these circles can be reached with a class IV movement; this is the desirable location for all procedures, specific equipment, and materials that the dental assistant will access.
The position of the assistant is important. The assistant is not facing the patient. Instead, the assistant is facing the back of the operatory so that the left hip is adjacent to the patient’s left shoulder (when assisting a right-handed doctor). This is important for ergonomics in terms of working around the vicinity of the chair. Of course, the left-handed doctor would employ a mirror-image seating configuration.
However, if the assistant’s left hip is at the patient’s left elbow, the dental assistant must lean to reach the oral cavity; an elbow of the assistant will invariably be placed on the bar of the stool for balance while the assistant leans. As a result, the assistant’s spine is rotated and the assistant may or will incur lower back pain and perhaps problems with internal organ displacement over many years.
Also, in this position, the assistant will not have a clear view to keep the operating field clear, and as a result, the assistant will not be able to anticipate the doctor’s needs.
However, with the assistant positioned properly relative to the patient and with their eye level preferably six to eight inches above the doctor’s eye level, the assistant will be able to fully participate in the procedure without compromising their physical health.
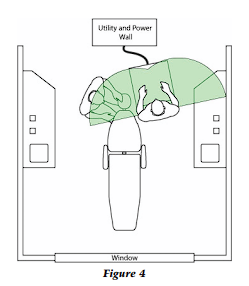
The primary workspace is the area encompassed by the two semicircles in front of the assistant (Fig 4). Instrument transfer as well as static and dynamic storage of instruments occurs in this area because instruments are easily retrievable and replaceable. There is drawer access for consumables but not for instruments; they belong on trays or cassettes.
Consumables may also be on a tray but supplies are readily available. During the course of the treatment, if a consumable from the primary instrument tray is depleted, the assistant can retrieve additional supplies from a drawer either by pick-up forceps or the use of a barrier on the drawer pull (such as a 4″ x 4″ gauge), which is very simple.
Therefore, it is desirable to install drawer pulls for operatory drawers. Metal drawer pulls are easy to disinfect as opposed to heavily routed ledges underneath the drawer that cannot be easily disinfected. In retrieving supplies from a drawer, the assistant can either use pick-up forceps, over-gloves, or gloves when necessary. Do not risk cross-contamination of instrumentation or puncture wounds by storing instruments in operatory drawers; all instruments should be in trays, tubs, or cassettes and stored in the central sterilization area.
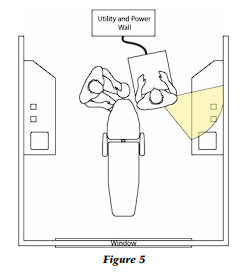
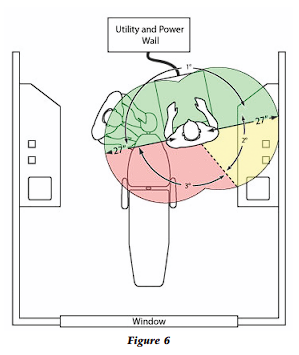
The secondary workspace (Fig. 5) is intended for mixing and temporary storage of backup tubs or additional procedure trays if more than two procedures will be performed with the same patient. Once the assistant rotates her stool, the secondary workspace functions just as the primary space. Tertiary areas (Fig. 6) should never be used because access requires a severe class five movement to retrieve anything in this area. Do not place anything in tertiary space that the dental assistant must retrieve, replace, or access during the procedure.
Now that we are aware of the functional dimensions associated with the assistant, we can ergonomically construct the dimensions of the dental operator.
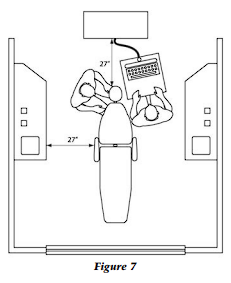
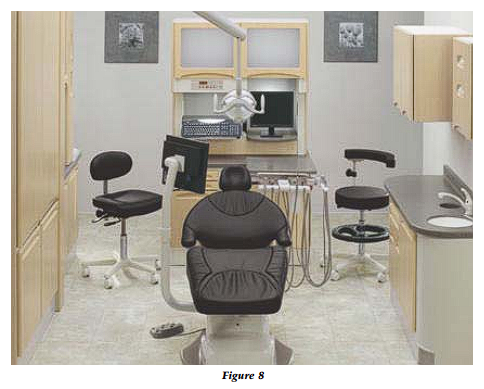
The distance from the back wall, separating the operatory from the clinical treatment hallway and otherwise known as the utility wall, to the head of the reclined chair should be 27 inches (Fig. 7). All small equipment usually used in the operatory should be stored on and in the utility wall (Fig. 8). The utility wall also facilitates the mounting and placement of the X-ray tube head behind the head of the patient.
This tube-head placement is a recommendation of dental radiologists simply due to the consistency of quality films generated when the X-ray tube head is placed behind the head of the patient. There are significantly fewer retakes because overlapping, elongations, and cone cuts are avoided with the centralized positioning of the tube head.
This does not imply that good radiographs cannot be obtained from the side or swing through cabinet delivery; it does mean that consistently more films will be retaken because of tube-head drift or difficulty in aligning the patient, film, and tube head due to the complete extension of the radiographic unit. There should be a 27-inch space from the vertical wall of the side cabinet to the arm of the dental chair so that the dental assistant can reach all functional ergonomic space (Fig. 7).
The majority of dental chairs are approximately six feet four inches long and 24- inches wide. When selecting a chair design for the operatory, it is desirable to use a narrow (24–27˝ wide), thin-backed chair that allows the doctor to come close to the patient and maintain a posture with the doctor’s elbows at his side. Of course, this positioning leads to the stool design that will put the doctor in the ergonomically correct seated position.
The thighs should be at approximately a 10º slope relative to the
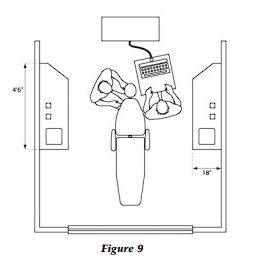
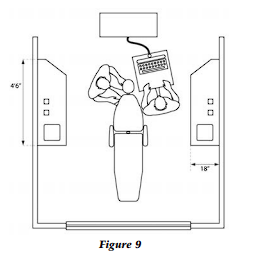
floor, and the pelvis should be canted downward toward the floor; this requires a stool with a seat that will tilt forward. Additionally, the front edge or tip of the stool should be beveled to prevent the embarrassment of circulation to the legs and lower body. So, purchase the ergonomically accessible (Fig. 9).
A key dimension of the operatory is the optimal six and a half feet for the width of the operatory from the vertical surface edge of one side cabinet to the other cabinet (Fig. 10). If the operatory space is wider than this distance, either the doctor or the assistant will not be able to reach the side cabinets without rising from the stool or attempting to slide the stool. This additional movement, of course, begets stress.
Also, this is a critical dimension because anything less than this will impede movement and any greater dimension will not allow the seated assistant to reach all areas of the side cabinet. The side cabinetry must have drawers and room for trash receptacles underneath the two trash drops for biohazardous materials and for noncontaminated trash. Additionally, there must be plumbing under the sink. These functional items require from 4 1/2 to 5 feet of linear counter footage for the side cabinet.
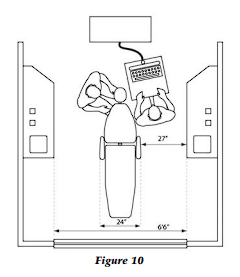
The side cabinet should be 18 inches deep and, therefore; the wall-to-wall width of the operatory will be nine and one-half feet. In order to achieve a fully ergonomic working environment, the dental chair width should not exceed approximately 27 inches.
The operatory should have a length of 10 feet from the back wall to the opening at the front and the inside surface of the utility or power wall (Fig. 11). With a six-foot-four-inch reclined chair in place, this dimension would provide one and a half feet of space at the foot of the chair and 27 inches from the head of the chair to the inside surface of the utility or power wall.
In designing a floor plan, codes such as the Americans with Disabilities Act, which dictates handicap minimum access, must be considered.
Compliance with the Code is achieved with the cited dimensions for the operatory in this book. For example, this code is one of the factors that determine the position of the head of the chair. The head of the reclined chair should be 27 inches from the utility wall and the vertical surface of the side cabinets are both 27 inches from the armrests of the chair.
With this configuration, a distance of two feet eight inches is created from the corner of the utility wall to the side cabinet. This “entrance dimension” is necessary and sufficient to meet the ADA Code for handicapped access, but as the wheelchair moves toward the chair, there is only 27 inches between the side cabinet and chair. However, two feet eight inches are required for handicapped access…resolve this dilemma by purchasing a chair with a foot release so that the chair can be rotated 30º to easily achieve handicapped/ wheelchair access (Fig. 12).
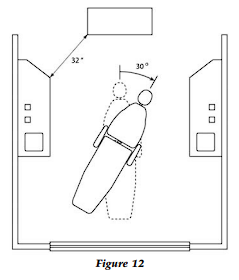
Having carefully planned for the code, it is suggested that the dental chairs are not drawn or indicated on the floor plan submitted to the municipal permitting/building office. The bureaucrat at the building department will measure the distance from the chair to the cabinet and determine that it is not two feet eight inches. The plans will be rejected and will need to be redrawn; this is very, very expensive. Explanations and discussions with the planning/permitting department are not very effective, so avoid the need for such discussion. No chairs, no problem.
The difficulty created by flared, thick-backed chairs is the displacement of the dental assistant and the doctor such that the ergonomic positioning of either person is very difficult. The doctor cannot place his legs sufficiently under the chair for close proximity to the patient, and the assistant cannot be positioned for clear visualization of the oral cavity because her left hip cannot be immediately next to the patient’s left shoulder.
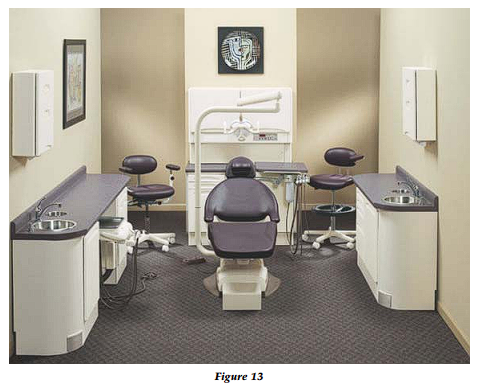
The desired shape of the dental chair that will facilitate comfortable ergonomic staff movement is thin and narrow (24-27˝). With the head and shoulder portion of the chair especially narrow, this will allow ergonomic access to the patient from the nine or three o’clock to the twelve o’clock positions (Fig. 13).
The operatory design is only the beginning. What about the rest of the office…central sterilization, laboratory, front desk, waiting area, radiography, consultation room, and any other areas? How can they be ergonomically designed to improve staff function? That is, how can the design of the office be used to increase productivity and decrease the emotional and physical stress of the doctor and staff?
For example, how many operatories are right for your practice? What is the optimal size of your waiting room? Is there a relationship between the size of central sterilization and the number of operatories in the practice?
These are all questions that must be answered correctly to create the optimal staff flow and office ergonomics; they are addressed in the book from which this article is excerpted, A Guide to Designing the Elegant Dental Office…The Largest Marketing Tool of Your Career.
Dr. Mark Tholen graduated from the University of Texas Dental School and U.T. Graduate School of Business with an MBA. He is the former CEO of a premier dental and medical office design firm and author of the book, A Guide to Designing the Elegant Dental Office…The Largest Marketing Tool of Your Career. He can be reached at marktholen2000@yahoo.com
All illustrations are courtesy of the University of Texas Department of Medical Illustration.
Copyright 2023 © Tholen Healthcare Environments | Privacy Policy